IVF treatment involves a team of doctors, embryologists, nurses and support staff. The advice and expertise of an embryologist makes a vital contribution to a patient’s treatment and experience.
Lucy Pullan is a trainee embryologist and has been working at Bourn Hall for four years. Her role includes egg collection, fertilisation assessment, embryo grading and transfer, semen analysis and providing feedback to the patients about their progress.
After her degree in human biology at Bristol Lucy worked in the histology department at Southend Hospital. She enjoyed the lab work there but wanted to have more patient contact – and now she has a job that she loves at Bourn Hall Norwich.
I love being a trainee embryologist
Reproductive science was one of the modules I had enjoyed during my degree, but it is quite a competitive field to get into. I was going to study a masters and went to the Bourn Hall Cambridge clinic for work experience. While I was there a job came up in the Norwich clinic as a practitioner, which gave me the practical skills of working in an embryology lab. Then Bourn Hall offered to train me to become a clinical embryologist, which was amazing timing. I relocated to Norwich and I love it up here.
I am a trainee while I am on my course, so a lot of my time is spent studying and training. I am allowed to do more of the lab aspect such as egg collections, semen analysis scoring of embryos and embryo transfers and freezing.
I don’t do ICSI yet (where the sperm is injected into an egg) but that is something which I will hopefully learn next year; you do have to be a bit more experienced for that.
One of my favourite parts of the work is going into theatre and telling the patient about their embryos. Face-to-face contact with the patient is limited but communication with patients both over the phone and through email is increasing, and it is really important to them.

Embryo grading is an important part of my job
We use a grading system to identify the embryos with the best potential for success. For example, we might say ‘you have five which are top quality, three which are good and two which are poorer’. If the patient wants more detail, we are always happy to explain the system and how each individual embryo is graded.
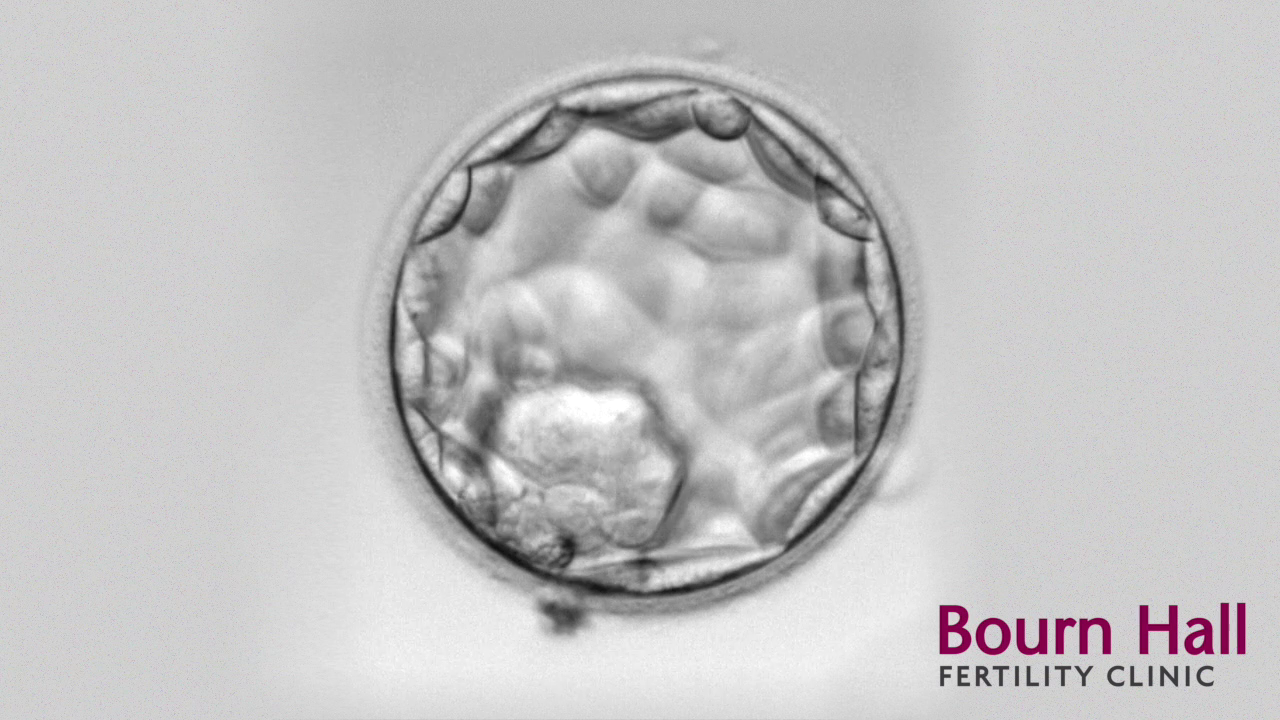
Embryo grading at an early stage of development can be subjective, which is why we aim to culture most embryos to the blastocyst stage.
The top-quality embryos are easier to score, it is when they start to get a bit poorer it is harder. If there is ever any doubt, we do check each other’s scores and although we may sometimes disagree on the actual grade, we always agree on which is number one and number two etc.
Sometimes there is just one embryo available, but if there are several there may a discussion to be had: will one embryo or two embryos be transferred? Are any of the embryos suitable for freezing? We give the patients and the doctor as much information as possible, so everyone can be involved in the decision.
Even embryos with a poor grade can become healthy babies, but if there is a choice, we want to pick the one most likely to succeed.
Sometimes we have a treatment cycle where the eggs fail to fertilise or the embryos have developed poorly – that might be an indicator as to why they haven’t been getting pregnant. You can learn a lot from a failed cycle, and we would make a note on the patient records, which the doctors can then use to improve the chances of success on a second cycle.

Egg collection and retrieval takes care
Tiny eggs, the size of pencil point, develop in fluid-filled follicles in the ovary. During egg retrieval, the doctor identifies follicles under ultrasound guidance, and a needle is used to aspirate the follicles, where the fluid is collected into little tubes.
The tubes containing eggs are brought into the embryology lab, which is literally a few steps away, and the follicular fluid is examined under a microscope to find the eggs. These are washed in culture media and placed in a dish in an incubator.
The eggs are surrounded by cumulus cells which makes the eggs easier to spot. If someone is having standard IVF we try to make this as natural as possible: so the eggs are mixed with the sperm in the dish and the cumulus cells removed the next morning when we perform the fertilization check. If the patient is having ICSI, we strip away the cumulus cells so we can see if the eggs are mature before we inject a sperm into it.
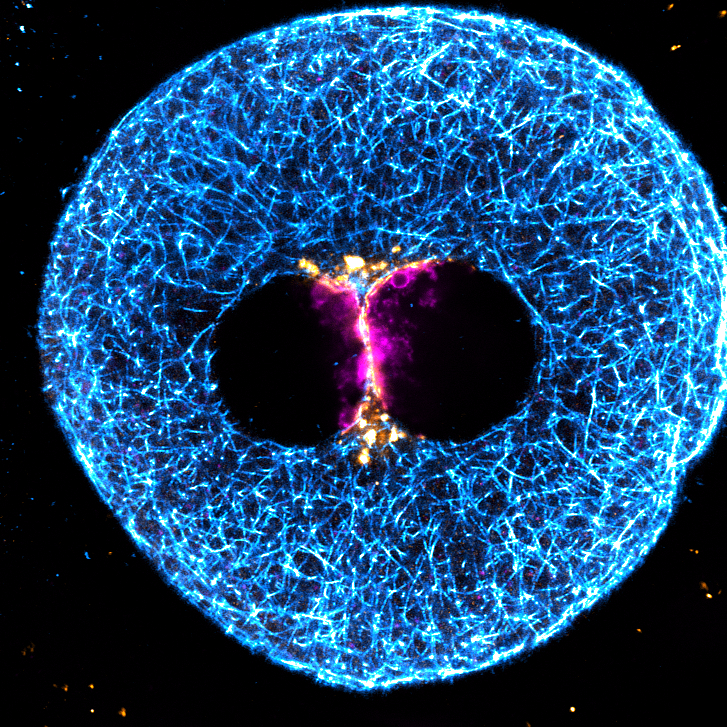
During the fertilisation check we are looking for two pro-nuclei – one is the maternal DNA and one is the paternal; you need just one of each, and at this stage, the embryo is just one cell.
Egg collection is classed as day zero; the fertilisation check happens on day one, then by day two we expect the embryos to have started dividing. Normally we would see between two and six cells at this stage.
This would continue, ideally, until day five when hopefully some embryos should reach blastocyst stage where the cells have differentiated, some becoming the baby and the remainder the placenta. If one of the embryos needs an extra day to reach blastocyst, that is not necessarily a bad thing; it got there, it was just a tiny bit slower.
Training to be an embryologist
Some of the other embryologists have worked in other clinics before coming to Bourn Hall, which is good because we learn from each other and every lab does things slightly differently.
As part of my training, we get to do an elective period and I am hoping to go and visit a couple of other clinics just see how they do things. Bourn Hall is good at supporting people to go to conferences and so on, which is a really good networking opportunity and a learning opportunity.

Research into surgical sperm retrieval
Dr Thanos has submitted a number of papers to the ACE conference and I am going to do a project as part of my training, so we may try and get that published.
For my project I am going to compare the outcomes between patients that have had surgical sperm retrievals (SSR) after a zero sperm count, known as azoospermia. This can occur when there is an obstruction in the tube, perhaps after a vasectomy reversal or because they are a carrier of the cystic fibrosis gene and don’t have a vas deferens. Or it can be non-obstructive, where there is something going on in the testicle. I am going to compare the two groups and look at the ICSI outcomes after using the sperm. Mr Oliver Wiseman, the andrologist and male fertility specialist at Bourn Hall, has been collecting data over the last ten years, which is great; it is a big dataset and that makes it more robust.
Being part of the Bourn Hall family
I love my job. I came into it for the patients and although for us it is our day-to-day, for them it is a huge thing and can be a difficult and emotional experience. I always try to really remember how daunting this can be for the patient and how I would feel if that was me getting advice on my embryos.
Pre-Covid some patients would bring their babies in which was special. We don’t get that at the moment sadly, but patients do send in thank you cards and pictures, and we pin them all on a baby board in our team room which is really lovely.

It just amazes me every day that we help make those little embryos that make babies!
When people ask me what I do and I say an embryologist most people don’t know what that is so they ask lots of questions, and that always really reminds me what I do and I think ‘oh, I am quite important!’. I do love it.