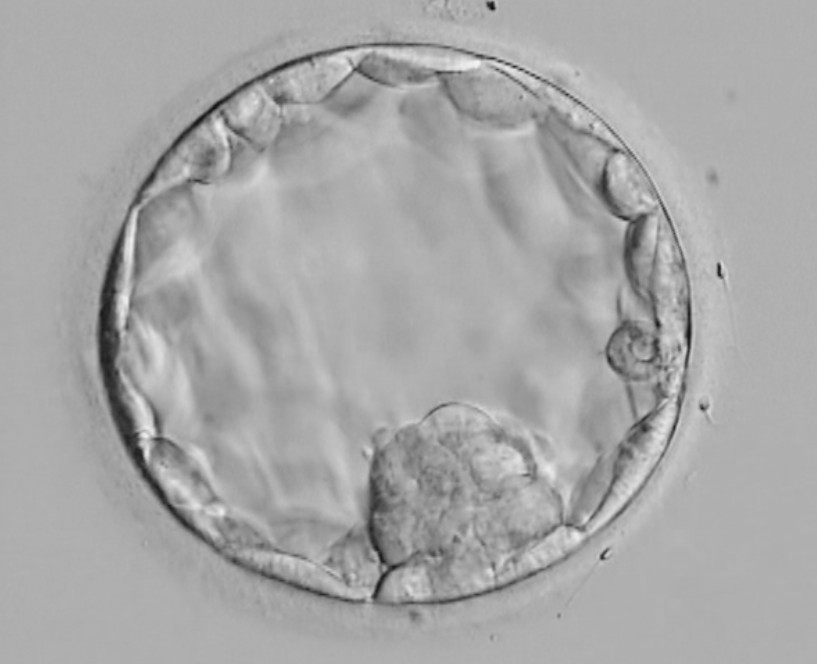
IVF success rates have improved over recent years and one factor is the increased use of blastocyst transfer, when the embryo is five days old. 45 per cent of our patients become pregnant following IVF with blastocyst transfer.
When the BBC visited Bourn Hall they were fascinated by a tour of embryology.
Lead embryologist Adam Burnley explained that in natural conception the embryo takes about five days to travel from the ovary down the fallopian tube, so it would have reached blastocyst – the stage when the cells in the embryo have started to differentiate so they can become different parts of the baby and the placenta – just as it reaches the womb.
If the above video does not play you can watch the video on YouTube here.
Boosting IVF success
 Blastocyst stage is reached during IVF treatment by allowing an embryo to develop in the incubator before it is transferred to the womb. The embryos are closely observed to check which are dividing rapidly and likely to reach blastocyst. Not all embryos are able to do this and the decision might be made to transfer an embryo earlier. This embryo would still be capable of resulting in a healthy pregnancy.
Blastocyst stage is reached during IVF treatment by allowing an embryo to develop in the incubator before it is transferred to the womb. The embryos are closely observed to check which are dividing rapidly and likely to reach blastocyst. Not all embryos are able to do this and the decision might be made to transfer an embryo earlier. This embryo would still be capable of resulting in a healthy pregnancy.
In addition to manual observations, which require the embryos to be taken from the incubator for viewing, Bourn Hall has invested in some new incubators fitted with the Eeva system. This is a video capture system that images the embryos every few minutes and uses a special algorithm to calculate which embryos are most likely to reach blastocyst.
Adam Burnley explained to Dr Chris Smith of the BBC’s Naked Scientists some of the benefits of this approach:
”In the lab we try to replicate as closely as possible the natural environment of the body. The big benefit of Eeva is that it allows us to monitor the embryos with very little disturbance. It also provides an objective assessment of the viability of the embryo which can be helpful when two embryos look identical or when an earlier transfer is required.”
Checking egg quality
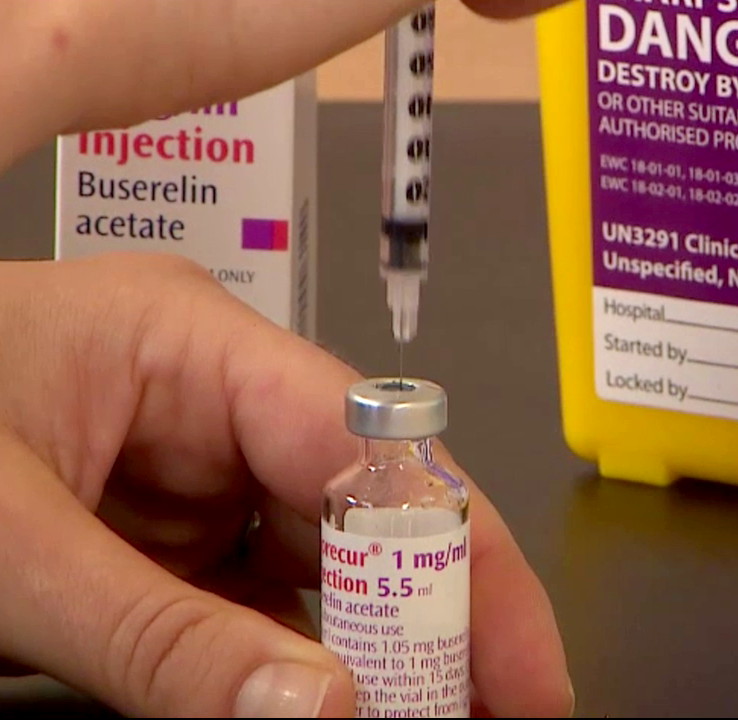
For patients concerned about their egg quality and likely response to stimulation drugs, the AMH (Anti-Mullerian Hormone) test, provided either as part of a suite of fertility tests or on its own, can provide some helpful information that can be used to advise about treatment options.
The AMH test gives an indication of the reserve pool of eggs left in the woman’s ovaries (not the exact number). This information is used to decide whether it would be worth attempting ovarian stimulation for egg collection and IVF.
Even if the AMH level is low, if other factors look good and the patient wants to try, then ovarian stimulation might still be possible although it may be necessary to use a higher dose of drugs.
These are some of the types of options that are discussed as part of the initial consultation. Patients can have all their fertility testing done at Bourn Hall, which means that they have continuity of care through every stage of their fertility journey.