Ben and Lucie were teenage sweethearts. Lucie runs a hairdressing salon from home and Ben runs his own plumbing and heating engineering business. They had been together seven years when they decided to start a family. Lucie was still only 22 so initially it was difficult to get help.

All I wanted was to be married with kids
“I always wanted to have children and we started to try. Then we went on holiday to Majorca and were just lying on the beach talking and I said ‘I think I want to get married before we bring children into the world. I want to have the same name as my children’.
“So, the following year in May 2015 we got married and started trying from then.
“It got to the point that I was doing everything. I’d got the app on my phone, I was checking my temperature, body discharge, everything. I always used to get ovulation cramps as well so I sort of knew when the time should have been right.
“It didn’t work basically.”
Getting advice led to investigative tests
The couple went to their GP for advice.
“I wasn’t taken seriously to begin with as I was so regular – every 28 days. Ben’s tests all came back fine so the doctors were a bit stumped, I guess.”
Lucie was referred to Peterborough Hospital for a HyCoSy test – this uses a dye to check that the tubes leading from the ovaries to the womb are all clear. This revealed Lucie had a blocked fallopian tube and she had an operation to see if it could be unblocked .
“The consultant said to me before the investigation ‘if we find something do you want us to do surgery’ and I agreed. They found I had got a blockage on my left fallopian tube, so they removed it there and then. They said ‘the fallopian tube is so tiny that trying to unblock it would probably cause more damage’.
“It was a bit of a shock; I thought ‘that’s it, I am never going to be able to have children'”.
Tests had uncovered ‘hidden’ fertility issue
“It was a hidden fertility issue. We may never have known about the blocked tube if we hadn’t gone for the tests at the hospital – as both our initial tests were fine.
“With only one fallopian tube, I thought I’d got a 50:50 chance. I was thinking I could be ovulating from the left side for six months and obviously nothing is going to happen. Actually, they told me that it wouldn’t halve my chances it was only like 20 per cent or something because of how you ovulate on different sides.
“They sent us away for six months to try naturally again. But we were thinking it was never going to happen, and trying just became a chore.”
Referral for IVF coincided with NHS funding cuts
Lucie and Ben were told they would need IVF, but then disaster struck as Cambridgeshire and Peterborough CCG announced it was cutting all funding for NHS treatment. (This was reinstated in 2021)
“When we heard about the NHS funding cuts panic hit,” says Lucie. “I was desperate for children. The thought of not ever becoming a parent was unbearable.
“We had a meeting at the hospital to discuss next steps; it was bit of a knife-edge, but because of the date of my operation we were told that we would still be eligible for funding.
“We had the letter to confirm this just two weeks before we started treatment – the same month that funding stopped!”

Starting on medication ahead of treatment
“At the time it seemed as though we were the only ones who couldn’t get pregnant, but we went for a seminar at Bourn Hall (this was before Covid) and there were about 20 couples, so we didn’t feel so alone.
“To be honest, the first injection was the worst. My husband always says I am such a strong-willed person but the thought of the injections was scary.
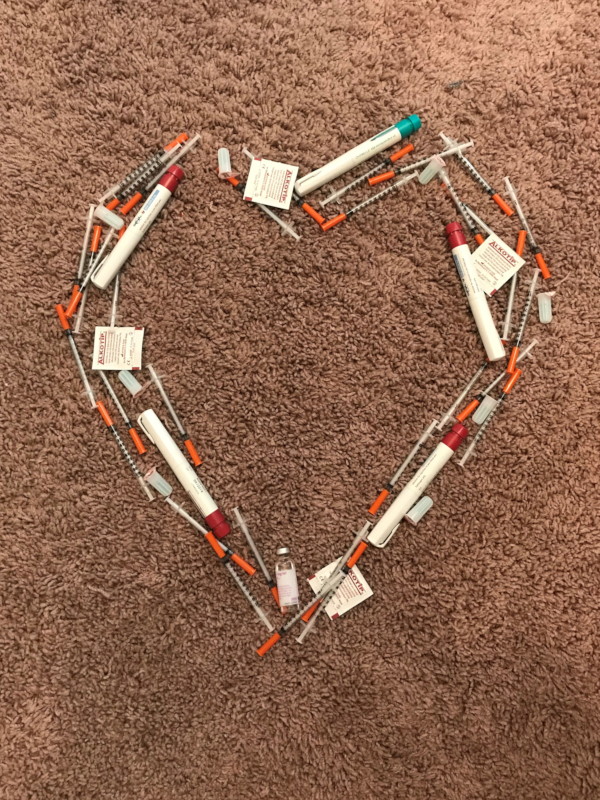
“I had my mum with me and she was saying ‘you know this is going to get you what you want, so you need to do it’. There were 60 injections, but after I had done the first one, I was like ‘I don’t know what I was worrying about’. Actually, it was fine.
“Medication puts you through a menopausal state and I remember waking up a few nights absolutely drenched in sweat.
“There were a couple of times I would get to the point of thinking ‘why me? Why can’t we just be like any normal couple and it just happen?’ But other than that my body felt quite well, to be honest.
“You have to keep the medication at a certain temperature and do the injections at a certain time. I went to a concert with my sister to see Jess Glynn. I just didn’t think about this when we booked the tickets and I suddenly wondered ‘how am I going to do my injections? It needs to be kept in the fridge?’ I remember going and buying a coolbag to keep it at a certain temperature and waiting in the car with my sister – so many things you don’t think about before you start treatment.”
Egg collection and fertilisation
The medication is to stimulate the ovaries to develop more than one mature egg.
“On the scan they could see 12 eggs developing. That is a good amount, a number they like to see. But when they went in to take them out they only managed to get four.
“It wasn’t very nice; they numb you and you are half conscious. It’s painful because everything inside is blown up so they can get out what they need. I remember a weight, like you get in the gym, pushing down on my stomach, obviously to try and move the ovaries and try to get as many eggs as they could. They got four eggs and then called me the next day to say two hadn’t fertilized.
“So I had two embryos which looked good. I was a bit disheartened because I thought ‘I have only got two and if they don’t work, I have got to do this all again’.
Transferring our embryo to its ‘natural habitat’
“When they talk about the embryos, they ideally want them to get to day five blastocyst stage, so I was worried when they called me and wanted me to go back in at day two.
“Did that mean I really had not got a chance? Were they just hoping for the best?
“But they told me that it was a really good embryo – they have got a scale (grading) and they told me that it was already developing to a six cell embryo and it had doubled and it was really strong. They said to get it back into its natural habitat was the best thing to try and make it work.
“The other embryo got to a day five blastocyst and was frozen.”
Will the embryo fall out?
“I remember asking them after embryo transfer if it was alright to stand up, would the embryo fall out?
“I had to go for a bridesmaid dress fitting for my friend that same day, and mum said it would take my mind off it. But I didn’t dare get off the chair until they said I was free to go. I thought ‘I don’t even want to risk doing a wee until I know I am pregnant’!
“It was a relief when Bourn Hall said I didn’t have to go home and rest, just do what my body was used to normally, because having bedrest wouldn’t make it work any better.
“So I went for the dress fitting and then to the pub afterwards and thought ‘I could actually be pregnant now!’ It was my little secret.”

The long wait before the pregnancy test
“I had to wait 12 days to do a test; that was awful, the waiting – and I had no symptoms that I was pregnant. Some people just know don’t they?
“I hadn’t even told Ben the test had to be done that day, I just thought if it was bad news I would need some time on my own, rather than people asking about the result.
“I remember I could hear him downstairs and I woke up and I couldn’t wait any longer. I heard him go off to work and did the test. The lines were so faint I wasn’t really sure. I had never had a positive test before, and I assumed it would just come up bold. Also, I had read that if you test too early you can get a positive result because your hormone levels are still high.
“I rang my mum; she said ‘I don’t know, it’s been 30 years since I have done a test, ring Bourn Hall and see what they say.
“I rang Bourn Hall and spoke to a nurse and said ‘I can see two lines but they are not bold’ and I can remember her saying to me ‘you are pregnant’ and I just burst into tears.
“In my lunch break I made Ben a card saying ‘you are going to be a dad’ for when he came home – he couldn’t believe it. I videoed him so that was really nice.
“I also phoned my mum and made her go and buy me some Clearblue tests just to be sure, because the lines were so faint. I did seven more tests over the next few days.”
She is here and we are parents at last
“I had a good pregnancy, and Alice-Mai was born at Hinchingbrooke Hospital on 23 August 2019, in five hours. I remember just looking at her; it was surreal. I hadn’t put anything up at home, not even the Moses basket – I didn’t want to tempt fate or anything.
“We just felt in a bubble – she was here and she was ours.”

Frozen embryo transfer and dreams of having second child
“There are five years between me and my sister and then eight years between me and my half-sister (I am the oldest) and I always said it was too big a gap – I wanted my children to be closer in age.
“Selfish as it sounds, my body was craving another child; I knew that I didn’t just want one. I was so lucky to get one but my mind and body knew I wanted two children.”
“We only had one frozen embryo left, and I had it in my head that the longer it was left it would lose its goodness. I knew this wouldn’t have happened because it was frozen, but I didn’t want to take the chance.

“Alice-Mai had just turned one when we went back to Bourn Hall – the day after her first birthday was my first injection.
“We had to pay for treatment as had used our allotted NHS-funded cycle, but Frozen Embryo Transfer is less expensive than full IVF. It is straightforward, with fewer injections as the embryo was already ‘made’ – it was just a case of preparing my body.
“I was worried it wouldn’t work, I got it into my head that this embryo wasn’t as strong. With fresh, you think it has got more chance, as it hasn’t been messed about with – it sounds silly: like food you freeze it and that sometimes takes the flavour away.
“Thawing day came. We got there and it had been thawed and it was fine to go – it was a similar grade to Alice-Mai.
“For the FET, I had to go on my own because of lockdown. Ben stayed at home with Alice-Mai and I took myself as no one was allowed in (partners are allowed into the clinic now). Ten days later I did the test to see if I was pregnant.
“I had bought some Clearblue tests this time and it was a lot clearer – part of me knew this time it had worked – I felt I knew.”

Science is amazing
“We were really lucky that the treatment worked first time both times. But it took us four or five years for us to get our children, and everything we had to do to get them. Now I have got them I think how lucky I am and forget what we have been through.
“Some people go through a lot of heartache, so I know now we were lucky.
“The science that goes in to it is amazing – I understand why it costs so much because of the technology and the science that is used, but it is sad for people who can’t afford it. I think everyone should get at least one round free, no matter the circumstances; if there is a medical issue people should be given at least one chance.
“Everyone was amazing at Bourn Hall, so friendly; I didn’t ever go in there thinking that I was’ just a number. At Bourn Hall they genuinely care and want the best for you right from the lady on reception to the doctors and the lab people – I remember the embryologist coming out and discussing the grades – everyone right through to lab wants the best for you.”







