“In my personal experience I’ve seen Pre-implantation Genetic Testing (PGT) help people from all walks of life,” says Katie Finch, Principal Embryologist at Bourn Hall’s Wickford clinic.
Katie explains in this blog how the PGT technique checks that the embryo has the right number of chromosomes and is only used when there is a concern that the resulting child might inherit an adverse medical condition.
Reducing risk
She explains who may benefit: “Couples who have a high risk of a specific condition and don’t want their children to inherit it, couples who have had an affected pregnancy and want to avoid the risks associated with pre-natal testing and the highly emotional decisions that go with a diagnosis, and those who want to avoid multiple transfers of unscreened blastocysts in order to achieve a healthy pregnancy sooner.
“PGT technology has come such a long way in the last decade and it is now more accurate and reliable.”

Katie obtained her bachelor’s degree in Medical Genetics before being awarded a BBSRC funded PhD scholarship, investigating genome organisation and pre-implantation genetic diagnosis at The University of Kent. With over 15 years’ experience in both NHS and private sector fertility services, she is a qualified Intracytoplasmic Sperm Injection (ICSI) and biopsy practitioner with a specialist interest in Pre-implantation Genetic Testing (PGT) and rare chromosome conditions.
Here Katie explains what PGT is, which patients may benefit and gives an update on the latest news about this technique.
Increasing chances of a healthy pregnancy
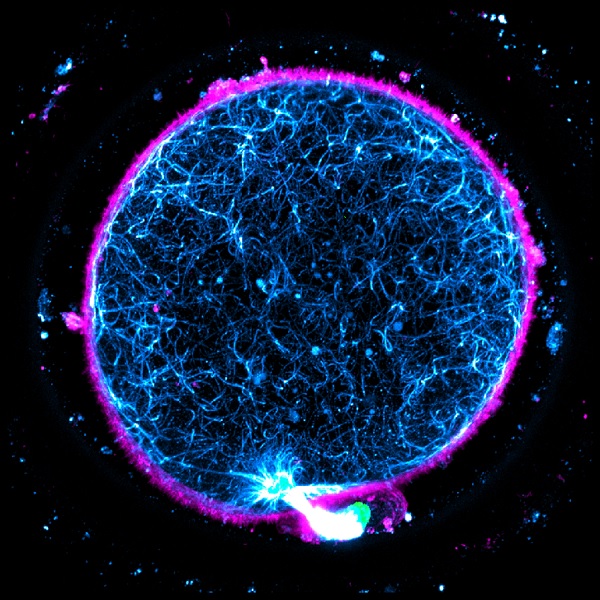
“Pre-implantation Genetic Testing (PGT) was first successfully used in 1989 to look at the chromosomes in embryos to see which were most likely to create a healthy pregnancy. The technique involves removing some of the cells within an embryo whilst it is developing in the lab. These cells can be tested to see if they contain:
- the correct number of chromosomes (Aneuploidy: PGT-A)
- chromosomes in the right sequence (Structural Rearrangements: PGT-SR)
- specific genes leading to a life-impairing condition (Monogenic/single gene conditions: PGT-M)
If the biopsied cells are reported as “normal”, the embryo which they came from can be replaced in an embryo transfer with the hope that it will lead to a healthy full term pregnancy.
Traffic light rating
The Human Fertilisation and Embryology Authority (HFEA) has developed a traffic light rating scheme, to help explain how much evidence there is for supplementary IVF techniques. These are procedures that are used in particular cases and as yet have limited clinical evidence to support their use.
Although the traffic light system gives day 5 PGT-A an amber rating this may soon be revised.
At this year’s European Society for Human Reproduction and Embryology (ESHRE) conference, it was agreed amongst an expert panel that PGT has been shown to reduce both miscarriage rate and the time to pregnancy (fewer cycles undertaken before a pregnancy was achieved).
Promising developments
Discussions from the ESHRE PGT consortium were summarised by Colleen Lynch, Training and Scientific Manager at Cooper Surgical. She reported that panel members discussed how it was incorrect to continue to label PGT-A as experimental and unproven, particularly in the light of new data arising from a number of published Randomised Controlled Trials including ESHRE’s own ESTEEM trial.
It was announced at the conference, that ESHRE is soon to publish new guidelines for PGT. Additionally, data was presented that demonstrated that blastocyst biopsy is not associated with adverse results in fresh or frozen IVF cycles.
The HFEA ‘traffic light’ system
Red
There is no evidence to say it is effective and safe.
Amber
There is a small amount or conflicting evidence that a treatment is effective and safe. Research should continue.
Green
There is more than one good quality trial showing that the treatment is effective and safe.
It should be noted that no techniques have yet been given a green rating by the HFEA.
Reducing chance of miscarriage
PGT can play an important role in a patient’s journey to parenthood. It can be used to help reach pregnancy sooner, reduce the chance of miscarriage or to help avoid an inherited known condition.
The test, known as PGS or PGT-A, is able to detect the number of chromosomes in an embryo.
Embryos that don’t have 23 pairs of chromosomes are unlikely to create a pregnancy, when they do; they have a significantly increased chance of miscarriage or the birth of a child with complex medical or educational needs such as those with Edwards’ or Down’s Syndrome. In a PGT-A cycle only “normal” (euploid) embryos are replaced, so whilst there are often fewer embryos to choose from, those that are replaced are more likely to created a full term healthy baby.”
Testing at Bourn Hall
At Bourn Hall, we offer Pre-implantation Genetic Testing for Aneuploidy (the correct number of chromosomes) at the blastocyst stage; the only clinic outside of London in the South of the UK offering this highly specialised technique. PGT-A can be beneficial to an array of patients not just by creating a healthy full term pregnancy, but also in avoiding the risks associated with invasive pre-natal tests and the challenging decisions that may need to be made following their outcome.